Life with new lungs is a blessed and interesting journey. Blessed by the gift of life given by my anonymous, wonderful donor family. And interesting because, well, it just is. Some folks might use the word challenging in the place of interesting, but everyone has challenges in their lives. Our challenges are just different, and an experience not shared by many, So I do find it interesting.
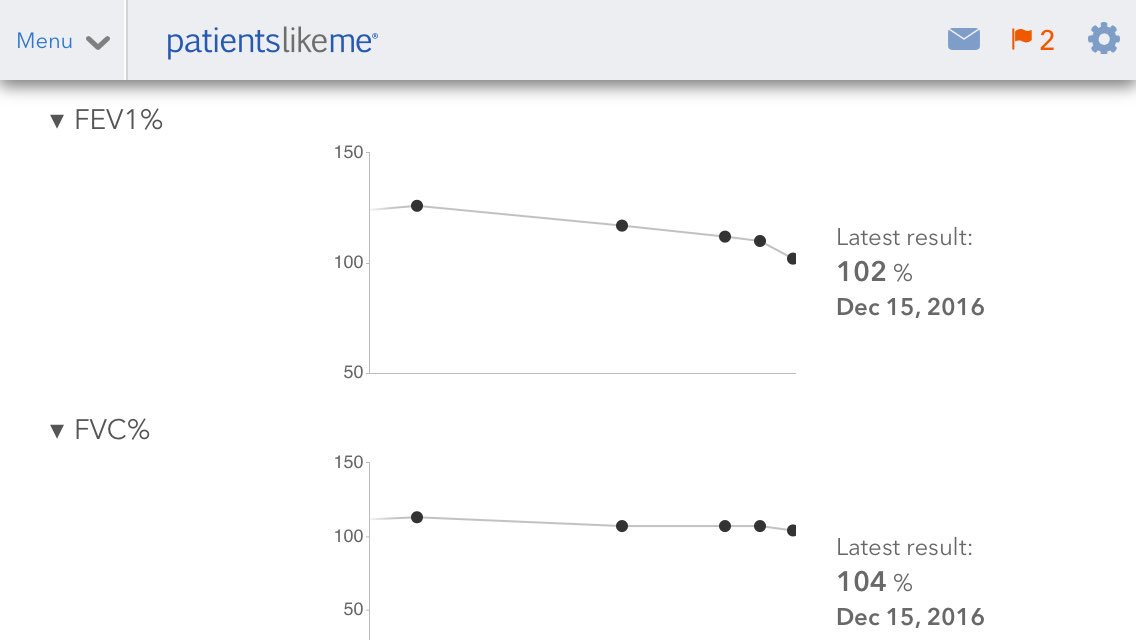
We take a few steps forward, then a couple steps back. Sometimes more than a couple in the wrong direction, but so far I've recovered and progressed after each setback. Over the past month or so my lung capacity has been slowly and consistently decreasing.
I feel good, and my routine exercise capacity hasn't been affected. I can tell there's something going on when I do higher intensity moves like continuous kettlebell swings, but for the most part it's business as usual.
I went to Clinic last week and found a rhinovirus in my sinuses, not the variation that would have had me admitted to the hospital for treatment. Just a silly little virus. The Team put me on a light prednisone taper. Just started at 40 mg/day. That's only 4 time my maintenance dose. It did stop the decline, but did not reverse the trend. Once the taper was done my capacity started dropping again.
So back to clinic today for the full workup. Labs, x-rays, and everything else look good. First thing tomorrow morning is a High Resolution CT Scan then off to the hospital for a bronchoscopy with a biopsy.
It's not a big deal really, I've had a lot of bronch's. Depending on which doctor does the procedure, they are sometimes the best sleep I get all month :)
I would like to make it between routine clinic visits without an issue more often. But as the Team Doc we saw today said "Some people are just really sensitive to viruses". That's me. My immune system can't handle a silly little virus so goes after the lungs.
I expect the end result of tomorrow's procedure will be a stronger prednisone taper, starting with at least 60 mg/day, probably higher. I'm sure the steroid will do its job and be back to normal in a couple of weeks.
This'll set my new fitness plan back a week or two, but that's not a big deal either. I expected a setback or three so started the program earlier than necessary. See.. planning, it is a good thing.
We all have setbacks, and when you are living with new lungs they can be expected and planned for. That's why our teams are so insistent about our taking our vitals every day, doing our home pulmonary function testing (PFT's) every day, and closely monitoring our own health in between clinic visits.
Update - 12/2/16
We were out the door at 6:15 this morning for the HRCT, then a quick trip across the street to the hospital for the bronchosopy.
The doctor who did the bronch is one of my favorites on the Team. She read the HRCT while going over what we were going to do during the bronch. The CT looked good, nothing out of the normal.
The bronch went very well and I'm home resting. We'll have the results next week and go on from there.
Update - 12/3/16
Electronic records are pretty awesome. This popped up in my in-box today.
FINDINGS
The vocal cords move appropriate to phonation.
The trachea is moist and unremarkable.
The main carina is sharp and non-displaced.
The right anastamosis was intact with no evidence of stenosis or dehiscense.
The RUL, RML and RLL were visualized. There were no lesions or secretions.
The left anastamosis was intact with no evidence of stenosis or dehiscense.
The LUL, lingula and LLL were visualized. There were no lesions and no secretions.
A BAL of the RML was performed. Specimen sent to micro.
A TBBx of the RLL were performed. Specimen sent to micro and pathology.
There was no noticeable bleeding at the end of the procedure.
There was no noticeable bleeding at the end of the procedure.
No evidence of pneumothorax post procedure
No complications
EBL < 5 cc
...RECOMMENDATIONS Follow cultures and biopsy resultsSo far so good.
Update - 12/8/16
CT results posted on MyChart this morning.
I have to admit that when I read "bronchiolitis obliterans", I kind of went into mental crisis mode. Bronchiolitis Obliterans Syndrome is a scary thing to mention to a lung transplant recipient.IMPRESSION:
1. A few scattered tiny nodular densities which may be inflammatory.
2. There is bibasilar mosaicism. The differential includes bronchiolitis obliterans
FOLLOW-UP RECOMMENDATIONS: Per clinical team.
Final Signed by...Narrative
EXAM: CT CHEST WO IV CONTRAST
HISTORY: 55 years old Male with lung transplant with declining lung function
TECHNIQUE: Volumetric data acquisition through the chest without IV contrast reconstructed as contiguous axial volume, MIP images, and multiplanar coronal and sagittal reconstructions per department protocol.
COMPARISON: 1/28/16
FINDINGS:
Lines and tubes: None.
Lungs and pleura: The trachea and central airways are patent. There is bronchial wall thickening. The lungs are remarkable for focal scarring and or atelectasis in the inferior lingula. There are no infiltrates or pleural effusions. There is patchy bibasilar groundglass.
So I sent off a message to my Transplant Coordinator and this is part of his reply:
Good Morning John,He continued with:
Your biopsies were perfect, A0B0 ( no cellular rejection or airway inflammation), all of the pathology / staining was unremarkable. Cultures were negative other than "normal respiratory tract flora". I had... review both your most recent and last CT chest images and he was "underwhelmed"...
...In my personal opinion your most recent CT looked better than the last.After a bit more conversation, I feel much better. Not yet time to break out my bottle of Sink the Bismark.
We also had to go to UTSW for a Dermatology follow up this morning. She had to freeze off a couple more spots on my head. That was a little irksome as I have recently completed three Blue Light Treatments. Hopefully we'll be able to get ahead of these issues with continued prevention. I really like our Dermatologist, she was able to see my Sweetie and I together in the same appointment. That really helps with scheduling the day. She's also been very helpful in getting my Sweetie some much needed non-derm related care.
So it's been and up down all around kind of day so far. A bright spot was getting a text from a transplant friend this morning right after I read the CT results. She was just checking in, and it came at the perfect time.
Now it's time to go swing my kettlebells. Kettlebells fix everything :)
Update - 12/15/15
Back to clinic for more tests and follow up with the team. My lung function has continued to drop as proven by the clinic Respiratory Therapist.
My annual exam is due next month, so we moved some of the tests up to today. Labs included 15 vials (half of my max draw) then I was off to ultrasound. Found that all of my pieces parts are still there. Then to Clinic for PFT's, 6MWT, and consultation with the Team.
We went over my CT's with a fine tooth comb. Yes, there is some air trapping, but all in all the lungs look as awesome as ever. The Six Minute Walk Test was pretty much the same as last year, which is as expected. My blood oxygen saturation stayed at 100% during the test, which is a wonderful thing.
End result of today's visit is that I'm going to be doing a IV Steroid Pulse at home over the next 3 days and have added another forever medication to my list. Azithromycin. It helps to prevent chronic rejection.
I'm pretty confident that the steroid pulse is going to do the trick. Just have to figure out how to do my kettlebell routine with an IV stuck in my arm :)
Update - 12/24/16
The steroid pulse has seemed to stop the decline, I've even recovered a little bit of lost lung function, but has settled out at about 15% lower than my max. I kind of feel bad being disturbed by this. I still have over a 5 liter FVC, which is amazing for an IPF transplant.
I've started a new forever antibiotic, Azithromycin. My Team also increased my Cellcept back up to 1000 mg twice/day. Seems my immune system is getting a little overactive.
I often wonder if all the things I do to stay healthy are a bit counterproductive. But they are working so far :)
Sorry to hear about the virus, John! I'm sure our superhero team will get you fixed right up. Take good care and let me know how it goes. I will keep you in my prayers.
ReplyDeleteYep, they'll get it lined out. The bronch looked good so a stronger prednisone taper will probably do the trick. Waiting for cultures to come back before starting a course of treatment.
Delete