The Cliff Notes version is that I had a Pulmonary Embolism (blood clot in my right lung). My Team decided to clear the clot using Thrombolysis to deliver medication via a catheter right to the clot in my lung. This resulted in a two day stay in the ICU and quickly cleared the clot. I spent a few more days in the hospital while they got me stabilized and am now back home. I'm a bit wrung out, but not much the worse for wear.
Now for the long version if you are interested.
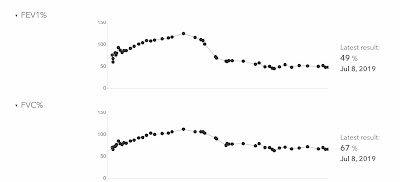
The day of my Pulmonary Embolism (PE) started out just like any other day. Woke up, took meds, did computer stuff and took more meds. I took a shower, shaved and all that stuff with no problems. It takes a little longer to get that routine done due to the rejection, but this did not take any longer or use more energy than usual. We went to lunch and on the way I stopped for gas. Other than a vagrant hassling me a couple of times, getting gas was issue free. We went to Raising Cane's Chicken Fingers for lunch, and this is where the issues started. I got very out of breath just walking from the car into the restaurant. I ordered and sat down. When I went to pick up our food, I could hardly make it back to the table I was so out of breath. I asked my Sweetie to get to-go boxes as I wanted to get the heck out of there. By the time she got back to the table I was feeling a little better and tried to eat. I got one chicken tender down before I had to go. By the time we got home, I felt better, but still a bit out of breath. I took my vitals and my pulse was elevated into the mid 120's, blood pressure was pretty much normal, and my spirometry was normal. The normal spiro confused me, I thought I was having an acute rejection episode going on. I called my Team and they said to come into the ER. It's been so long that I've spent an overnight in the hospital that I didn't have a go bag ready. I went to get some stuff gathered and started having a really hard time. My heart rate went up to over 150 and I was scary out of breath. There was no way I could drive so called 911. The 911 operator was awesome. Lots of people can't understand me over the phone in the best of times, she got everything perfect, the first time. You may be wondering why my wife wasn't helping me more, she has Alzheimer's and was doing her best to keep me comfortable and help out. When the ambulance and fire truck arrived, I explained that I had to go to UT Southwestern and asked if my Sweetie could ride with us. They said yes to both which took a huge load off of my mind.
When we got to the ER they did the routine ER stuff. My team had already been in contact with the ER doctor and they were ready for me. I was sent for a CT of my lungs with contrast fairly quickly. My daily at-home vitals and spirometry, and the data I got prior to calling the ambulance, helped them narrow down the possible issues quickly and I did not have to have a bronchoscopy to rule out acute rejection. The CT Scan showed:
There is an acute branching moderate-sized pulmonary embolus in the lateral and posterobasilar segmental arterial branches of the right lower lobe.Basically a blood clot in the lower lobe of my right lung. While in the ER we did an ultrasound of my legs to check for DVT blood clots in my legs. There were none. A room opened up for me and I left the ER for the 10th Floor. The 10th floor at UTSW is my home away from home.
Since I'm a lung transplant recipient, it is important that we quickly clear the clot. I was placed on an IV of Heparin and scheduled for Thrombolysis. Basically a catheter was inserted into my Jugular Vein, through my heart and into my Pulmonary Artery. The catheter was guided to the clot so medication could be administered right on the clot. The medication (tPA) was delivered through the catheter and Heparin was delivered via a sheath around the catheter. Now comes the rough part of this episode.
I was transferred from surgery to the ICU with my own nurse and everything. The major concern while receiving this clot buster medication is bleeding. Bleeding can happen anywhere so I was pretty much continuously monitored. Every half hour I had to answer questions about where I was at, what month/year it was... for signs of bleeding in my brain. All this time I am a bit out of breath and I have to admit that panic/anxiety tried to take over a couple of times through the night. An Ultrasound Tech came in to check for clots in my arms and shoulders and this really helped to break the cycle of panic and I was able to keep it from taking over. I was scheduled for them to go in and see how the clot was doing first thing in the morning. About an hour before I was supposed to go down for the procedure, I experienced severe nausea. Dry heaving over and over again. The regular anti nausea med didn't help much, but the second one took care of the issue and I was fine by the time I got back to surgery. When they went in to look at the clot it was gone so they were able to remove the catheter. That was a huge relief. One more night in the ICU for monitoring then I was back on the floor.
The goal when I got back on the floor was to get my Warfarin dose right to keep my INR in the therapeutic range.
From ambulance ride to ride home was Saturday to Saturday. I have a new med and new labs, but I'm not much worse for wear.
Like Skillet sings in the song "You Ain't Ready":
"What doesn't kill me makes me who I am"I am very thankful to my donor family for the gift of these lungs that have done me so well for the past 5 years, for my Team who work so hard to keep me healthy, and to the Lord for making everything right.